Last Updated on August 16, 2024 by Alexander Sennuga
Diabetic eating disorders are a complex and often misunderstood issue that affects many individuals living with diabetes. The intricate relationship between diabetes management and food consumption can lead to various challenges, including disordered eating patterns. In this comprehensive guide, we’ll explore the different aspects of diabetic eating disorders, their impact on health, and strategies for managing these conditions effectively.
What is Diabulimia?

Diabulimia is a term used to describe an eating disorder specific to people with Type 1 diabetes. It involves deliberately reducing or omitting insulin doses to lose weight. This dangerous practice can lead to severe health complications and is often overlooked in discussions about eating disorders.
Learn more about diabulimia from the National Eating Disorders Association
How Diabetes Affects Eating Habits
Diabetes significantly impacts an individual’s relationship with food. The constant need to monitor blood sugar levels, count carbohydrates, and adjust insulin doses can create a hyper-awareness of food consumption. This heightened focus on eating can sometimes lead to disordered eating patterns or full-blown eating disorders.
Some ways diabetes affects eating include:
Strict meal planning and timing
Carbohydrate counting and restriction
Fear of certain foods that may spike blood sugar
Guilt associated with “forbidden” foods
Frequent blood sugar checks before and after meals
The Connection Between Diabetes and ARFID

Avoidant/Restrictive Food Intake Disorder (ARFID) is an eating disorder characterized by extremely picky eating and a lack of interest in food. While there isn’t a direct causal link between diabetes and ARFID, the restrictive nature of diabetes management can sometimes contribute to the development of ARFID-like behaviors.
Diabetics may develop ARFID-like symptoms due to:
Fear of certain foods affecting blood sugar levels
Anxiety about trying new foods
Sensory sensitivities exacerbated by diabetes-related stress
The Dangers of Diabulimia: Mortality Rates and Health Risks
Diabulimia is a life-threatening condition with significant health risks. While exact mortality rates are challenging to determine due to underreporting and misdiagnosis, studies suggest that individuals with Type 1 diabetes who engage in insulin manipulation have a much higher risk of complications and premature death.
Health risks associated with diabulimia include:
Diabetic ketoacidosis (DKA)
Kidney damage
Nerve damage (neuropathy)
Vision problems or blindness
Cardiovascular disease
Read more about the health risks of diabulimia in this medical journal article.
Understanding Insulin Belly Fat
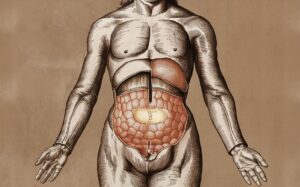
“Insulin belly fat” refers to the tendency of some people with diabetes to accumulate fat around their midsection. This occurs due to a combination of factors, including:
Insulin resistance
High insulin levels in the body
Hormonal imbalances
Poor blood sugar control
While not exclusive to people with diabetes, insulin belly fat is more common in this population due to the nature of the condition and its treatment.
Diabetes and Weight Gain: Focus on the Stomach
Weight gain, particularly around the stomach area, is a common concern for many people with diabetes. This is often due to:
Insulin’s effect on fat storage
Increased appetite due to blood sugar fluctuations
Reduced physical activity due to diabetes complications
Side effects of certain diabetes medications
To combat stomach fat gain, focus on:
Balanced, portion-controlled meals
Stress management
Working closely with your healthcare team to optimize diabetes management
Foods to Avoid for Diabetics in Diabetic Eating Disorders
Diabetics need to be careful about what they eat to keep their blood sugar levels in check. Some foods can cause big spikes in blood sugar and should be avoided. Sugary drinks like soda and fruit juices are a no-go, as they contain lots of added sugar.
White bread, pasta, and rice are also best left off the plate, as they quickly turn into sugar in the body. Fried foods and fatty meats can lead to weight gain and make it harder to control blood sugar.
Sweets like candy, cookies, and cakes are obvious culprits and should be limited. Even seemingly healthy foods like dried fruit can be problematic due to their concentrated sugar content. Instead, diabetics should focus on eating whole grains, lean proteins, vegetables, and small portions of fresh fruit to help manage their condition.
While there’s no one-size-fits-all approach to diabetes nutrition, certain foods are generally considered less beneficial for blood sugar control. Here are five foods that diabetics might want to limit or avoid:
Sugary beverages (soda, sweetened tea, fruit juices)
Processed snack foods (chips, crackers, pretzels)
White bread and other refined grains
Full-fat dairy products
Fried foods
Remember, complete elimination of these foods isn’t necessary. The key is moderation and working with a registered dietitian to create a balanced meal plan that fits your needs.
Challenges Diabetics Face with Eating
Living with diabetes comes with many challenges, especially when it comes to eating. People with diabetes must constantly watch what they eat to keep their blood sugar levels in check.
This means carefully planning meals, counting carbohydrates, and often avoiding foods they enjoy. Eating out can be particularly tricky, as it’s harder to know exactly what’s in restaurant meals.
Diabetics also need to be mindful of portion sizes and timing their meals to match their medication. Sometimes, they may feel left out during social gatherings centered around food. Moreover, the need to frequently monitor blood sugar levels before and after eating can be tiring and stressful.
Despite these difficulties, many diabetics learn to manage their condition well with proper education and support from healthcare providers and loved ones.
Many people with diabetes struggle with various aspects of eating. Some common challenges include:
Constant carbohydrate counting and meal planning
Fear of hypoglycemia or hyperglycemia after eating
Social situations involving food
Emotional eating triggered by diabetes-related stress
Difficulty finding suitable options when dining out
These challenges can sometimes lead to disordered eating patterns or full-blown eating disorders if not addressed properly.
The Impact of Overeating on Diabetics

Overeating can be very harmful to people with diabetes. When diabetics eat too much, their blood sugar levels can rise quickly. This makes it hard for their bodies to control blood sugar, which is already a challenge for them.
Eating more than needed can also lead to weight gain, which can make diabetes worse. Too much food can strain the digestive system and cause discomfort.
For diabetics, it’s crucial to eat balanced meals and stick to a healthy diet plan. Overeating can undo the benefits of medication and lifestyle changes they’ve made to manage their condition.
It’s important for diabetics to be mindful of portion sizes and to eat regular, well-planned meals to keep their blood sugar stable and maintain overall health.
When a diabetic person overeats, especially carbohydrate-rich foods, it can lead to:
Rapid blood sugar spikes
Difficulty in insulin dosing
Increased risk of hyperglycemia
Long-term complications of frequent overeating occur
Strategies to prevent overeating include:
Eating mindfully and slowly
Using smaller plates
Planning meals in advance
Managing stress through non-food-related activities
Can Starvation Trigger Diabetes?
While starvation itself doesn’t directly cause diabetes, severe calorie restriction, and malnutrition can impact insulin sensitivity and glucose metabolism. In some cases, this can contribute to the development of type 2 diabetes or exacerbate existing diabetes.
Starvation can affect diabetes risk through:
Disruption of normal hormonal balance
Muscle breakdown, which can impact insulin sensitivity
Stress on the body potentially affects blood sugar regulation
It’s crucial to maintain a balanced, nutritious diet for overall health and diabetes prevention or management.
Weight Loss for Insulin Users

Losing weight while using insulin can be challenging but is certainly possible. Here are some strategies that can help:
Work with your healthcare team to adjust insulin doses
Focus on portion control rather than strict dieting
Incorporate regular physical activity
Choose complex carbohydrates over simple sugars
Stay hydrated and get adequate sleep
Remember, rapid weight loss is not recommended. Aim for slow, steady weight loss of 1-2 pounds per week.
Debunking Myths About Diabulimia
Several misconceptions about diabulimia need to be addressed:
Myth 1: Diabulimia only affects young women.
Truth: While more common in young women, diabulimia can affect anyone with Type 1 diabetes, regardless of age or gender.
Myth 2: Diabulimia is just a phase and not a serious condition.
Truth: Diabulimia is a severe and life-threatening eating disorder that requires professional treatment.
Myth 3: You can’t have diabulimia if you’re not underweight.
Truth: Diabulimia can affect individuals at any weight, and weight is not a reliable indicator of the disorder’s severity.
The Role of Insulin in Digestion

Insulin plays a crucial role in the digestion and metabolism of food. When you eat:
Blood sugar levels rise as food is digested
The pancreas releases insulin in response to this rise
Insulin helps cells absorb glucose from the bloodstream
Excess glucose is stored in the liver and muscles as glycogen
For people with diabetes, this process is disrupted, necessitating careful management of food intake and insulin dosing.
Conclusion
Understanding diabetic eating disorders is crucial for both individuals living with diabetes and healthcare professionals. By recognizing the complex relationship between diabetes and food, we can work towards better management strategies and support systems.
If you or someone you know is struggling with a diabetic eating disorder, don’t hesitate to seek professional help. Remember, a balanced approach to diabetes management, including a healthy relationship with food, is key to long-term health and well-being.

