Last Updated on August 16, 2024 by Alexander Sennuga
It may not be a complete exercise to just discuss the general signs and symptoms of diabetes. The signs of diabetes in women need a separate discussion.
These diabetes symptoms in women are the same regardless of the geographical origin of the woman.
In other words, it does not matter if the woman is American or African.
Common Symptoms of Diabetes
Regardless of gender, there are several common symptoms of diabetes that women should be aware of. These symptoms include:
- Increased thirst
- Frequent urination
- Fatigue and weakness
- Unexplained weight loss or gain
- Blurred vision
- Slow-healing wounds
- Tingling or numbness in the hands and feet
- Recurring infections, such as urinary tract infections and yeast infections
Unique Signs of Diabetes in Women:
1. Vaginal and Oral infections

The high glucose level in women can cause a fungal infection called Candida albicans. One type of this infection is the formation of near-white coatings on the tongue as oral thrush.
A vaginal infection (1, 2) is the other type of Candida albicans. It affects women in an isolated case or combined form around the vagina They may experience soreness, itching, pain when having sex, or vaginal discharge.
2. Urinary Tract Infections (UTI)
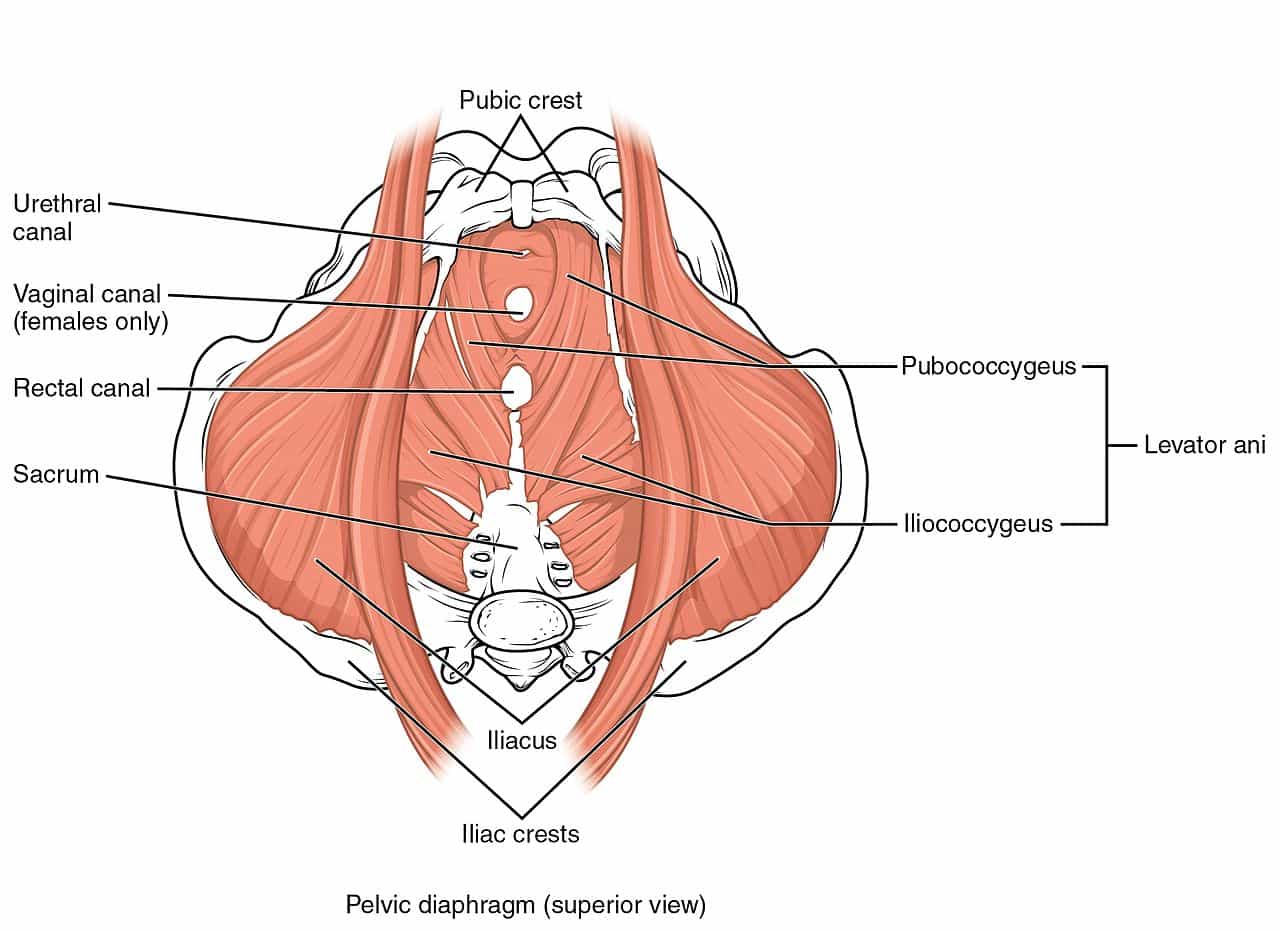
One of the diabetes symptoms in women is urinary tract infection (UTI) (1, 3). The woman starts noticing pains or a burning sensation and cloudy urine when urinating.
This is the result of bacteria gaining entry into the urinary tract without restriction. It then starts to grow until it causes infection.
3. Reduced Sexual Drive

Sexual dysfunction refers to difficulties or problems that individuals may experience in their sexual lives. It can encompass a range of issues that impact sexual desire, arousal, or satisfaction. Women with diabetes may be more prone to experiencing sexual dysfunction due to the physiological and psychological effects of the condition.
Diabetes can affect sexual health in various ways, leading to sexual dysfunction in women. Here are some factors to consider:
- Nerve Damage (Neuropathy): High blood sugar levels over an extended period can cause damage to nerves throughout the body, including those responsible for sexual sensation. This can lead to a decrease in sensitivity, making it more challenging to experience pleasure or achieve orgasm.
- Vascular Problems: Diabetes can affect blood circulation and impair the blood flow to the genital area. Reduced blood flow may result in decreased lubrication, making intercourse uncomfortable or painful.
- Hormonal Imbalances: Women with diabetes may experience hormonal imbalances, including fluctuations in estrogen and testosterone levels. These imbalances can affect sexual desire and arousal.
- Psychological Factors: Living with a chronic condition like diabetes can lead to psychological stress, anxiety, or depression. These emotional factors can contribute to reduced sexual desire or interest, affecting sexual function and satisfaction.
4. Polycystic Ovary Syndrome (PCOS)
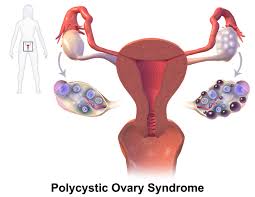
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder that affects many women of reproductive age. It is characterized by enlarged ovaries containing small cysts, hormonal imbalances, and symptoms such as irregular periods, excessive hair growth (hirsutism), and acne.
PCOS and diabetes have a close relationship. Research has shown that women with PCOS have an increased risk of developing type 2 diabetes later in life. In fact, it is estimated that approximately half of women with PCOS will develop diabetes or prediabetes by the age of 40.
The exact link between PCOS and diabetes is not fully understood, but insulin resistance plays a significant role. Insulin resistance occurs when the body’s cells do not respond properly to insulin, leading to elevated blood sugar levels. This can eventually lead to the development of type 2 diabetes.
Women with PCOS often have higher levels of insulin due to insulin resistance. The elevated insulin levels stimulate the ovaries to produce excess androgen hormones, such as testosterone. These hormonal imbalances contribute to the symptoms associated with PCOS, including irregular menstrual cycles, fertility issues, and the development of cysts on the ovaries.
Insulin resistance in PCOS also affects the body’s ability to regulate blood sugar levels effectively. Over time, this can lead to the development of diabetes if left unmanaged. Therefore, women with PCOS should be vigilant in monitoring their blood sugar levels and adopting healthy lifestyle habits to reduce the risk of diabetes.
The situations of hormonal imbalance in women are different from the situations of men. Thus it is important that every woman is aware of these signs, which may signal impending diabetes.
5. Gestational Diabetes in Pregnancy
Gestational diabetes is a type of diabetes that develops during pregnancy. It occurs when the body is unable to produce enough insulin to meet the increased demands of pregnancy, resulting in high blood sugar levels. This condition usually develops around the 24th to 28th week of pregnancy and typically resolves after childbirth. However, it requires careful monitoring and management to ensure the well-being of both the mother and the baby.
Here are some key points to understand about gestational diabetes:
- Risk Factors: Certain factors increase the risk of developing gestational diabetes, including being overweight or obese before pregnancy, having a family history of diabetes, being older than 25 years, having previously given birth to a large baby, and belonging to certain ethnic groups such as Hispanic, African American, or Asian.
- Importance of Screening: All pregnant women should undergo screening for gestational diabetes between the 24th and 28th week of pregnancy. The screening involves a glucose challenge test, where the woman drinks a sugary solution, followed by a blood test to measure blood sugar levels. If the results are abnormal, further testing, such as an oral glucose tolerance test, may be required to confirm the diagnosis.
- Effects on the Mother: Gestational diabetes can increase the risk of complications for the mother. It may lead to high blood pressure (preeclampsia), an increased likelihood of requiring a cesarean section, and an increased risk of developing type 2 diabetes later in life. Proper management of blood sugar levels during pregnancy helps reduce these risks.
- Effects on the Baby: When a pregnant woman has gestational diabetes, the baby is exposed to higher levels of glucose. This can lead to various complications, such as excessive growth (macrosomia), which may result in difficulties during delivery. The baby may also be at risk of low blood sugar (hypoglycemia) after birth and have an increased likelihood of developing obesity and type 2 diabetes later in life.
- Management and Treatment: Women diagnosed with gestational diabetes should work closely with their healthcare team to manage the condition effectively. This typically involves making dietary adjustments, engaging in regular physical activity, monitoring blood sugar levels, and, in some cases, using insulin or other medications. Regular prenatal check-ups, including fetal monitoring and ultrasounds, are essential to monitor the baby’s growth and well-being.
- Postpartum Care: After delivery, blood sugar levels usually return to normal. However, women who have had gestational diabetes are at an increased risk of developing type 2 diabetes in the future. Therefore, it is crucial to undergo postpartum screening and adopt a healthy lifestyle to reduce the risk of developing diabetes later in life.
Gestational diabetes requires proactive management to ensure a healthy pregnancy and reduce the risk of complications for both the mother and the baby. With proper medical care, lifestyle modifications, and close monitoring, women with gestational diabetes can have successful pregnancies and deliver healthy babies.
If you have been diagnosed with gestational diabetes, follow your healthcare provider’s recommendations, attend regular check-ups, and reach out for support when needed. The guidance of healthcare professionals will help you navigate this condition and promote the best possible outcomes for you and your baby.
Conclusion
Being aware of the signs of diabetes in women is crucial for early detection and effective management of the condition. Increased urination, excessive thirst, unexplained weight loss or gain, fatigue, frequent infections, changes in the menstrual cycle, sexual dysfunction, and the correlation with gestational diabetes and PCOS are all important factors to consider.
By recognizing these signs, women can take proactive steps to maintain their health, prevent complications, and lead fulfilling lives
Please share any other signs of diabetes in women using the comments form.
FAQ
- Q: Can diabetes be cured? A: While there is no known cure for diabetes, it can be effectively managed through lifestyle modifications, medication, and regular monitoring of blood sugar levels.
- Q: Are women more prone to diabetes than men? A: Both men and women can develop diabetes, but some specific symptoms and conditions like gestational diabetes and PCOS make women more susceptible to certain types of diabetes.
- Q: What should I do if I suspect I have diabetes? A: If you suspect you have diabetes or are experiencing any symptoms mentioned in this article, it is important to consult with a healthcare professional for proper diagnosis and guidance.
- Q: Can a healthy diet and exercise prevent diabetes? A: Adopting a healthy diet and engaging in regular exercise can significantly reduce the risk of developing type 2 diabetes. It is crucial to maintain a balanced lifestyle to promote overall well-being.
- Q: Is diabetes hereditary? A: While genetics can play a role in the development of diabetes, lifestyle factors also greatly influence the risk. Having a family history of diabetes may increase the likelihood of developing the condition, but it is not a guarantee.
Very Important: PLEASE note that all information provided on this site is for educational purposes only. They should not be used for medical advice, diagnosis, or treatment. So, please consult with your doctor and/or registered dietitian or nutritionist for any professional advice before applying any of the information on your health issues.

