Last Updated on January 30, 2024 by Alexander Sennuga

Understanding Diabetes
Diabetes, a persistent health challenge, disrupts the normal process by which your body transforms food into energy. When we eat, most of the food is broken down into sugar (also called glucose) and released into our bloodstream. Our pancreas makes a hormone called insulin, which acts as a key to letting the blood sugar into our body’s cells for use as energy
Two primary forms of diabetes exist: Type 1 and Type 2.
Type 1 diabetes is an autoimmune condition where the body does not produce insulin because the immune system attacks and destroys the cells in the pancreas that make insulin. Individuals diagnosed with type 1 diabetes must administer insulin daily for their survival.
Type 2 diabetes, which is far more common, occurs when your body becomes resistant to insulin or when the pancreas is unable to produce enough insulin. Unlike Type 1, Type 2 diabetes can be managed and even prevented with a healthy lifestyle.
Understanding the link between diabetes and skin conditions is crucial, as diabetes can have many effects on the skin, and skin conditions can be the first sign that a person has diabetes. In the following sections, we will explore the various skin conditions that can occur in people with diabetes and how to manage them.
Understanding Skin Conditions
Skin conditions, or dermatological disorders, are a broad range of issues that affect the skin. They can range from mild conditions such as acne and eczema to more severe conditions like psoriasis and skin cancer.
Skin conditions can have various causes, including genetic factors, immune system problems, infections, and environmental factors. They can cause symptoms like redness, itching, pain, and changes in skin colour or texture.
In the context of our focus keyword, “Diabetes and Skin Conditions,” it’s important to note that people with diabetes are more likely to experience certain skin conditions due to the body’s high blood sugar levels affecting the skin’s health.
In the following sections, we will delve deeper into the link between diabetes and skin conditions, exploring common skin conditions that people with diabetes may experience and how to prevent and treat these conditions.
The Connection Between Diabetes and Skin Conditions
Diabetes and skin conditions are interconnected in several ways. High blood sugar levels, a characteristic of diabetes, can lead to dry skin and slow the body’s healing process. This makes the skin more susceptible to infections and skin conditions.
Moreover, some skin conditions are more common in people with diabetes. For instance, bacterial and fungal infections are more frequent due to the body’s reduced ability to fight off harmful bacteria and fungi.
In addition, there are skin conditions that are unique to people with diabetes. These include diabetic dermopathy, necrobiosis lipoidica diabeticorum, and diabetic blisters
Understanding the connection between diabetes and skin conditions can help in early detection and treatment. Sometimes, skin problems are the first noticeable signs that a person has diabetes.
In the following sections, we will delve deeper into the common skin conditions that people with diabetes may experience, and how to prevent and treat these conditions.
Common Skin Conditions in People with Diabetes
People with diabetes are more susceptible to certain skin conditions due to the effects of high blood sugar levels on the skin. Here are some of the most common skin conditions that people with diabetes may experience:
- Diabetic dermopathy: This condition appears as light brown, scaly patches on the skin, often on the front of the legs. It’s harmless and doesn’t need treatment.

- Necrobiosis Lipoidica Diabeticorum (NLD): NLD causes spots similar to diabetic dermopathy, but they’re larger and deeper. The spots are shiny, with a red or violet border. They can be itchy and painful.
- Diabetic Blisters (Bullosis diabeticorum): In rare cases, people with diabetes develop blisters that resemble burn blisters. These blisters may appear on the digits, palms, toes, soles, shanks, or lower arms.

- Acanthosis Nigricans: This is a condition that makes the skin in the body’s folds and creases dark, thick, and velvety. This skin change usually occurs in people who are obese and have diabetes.
- Skin Infections: People with diabetes are more prone to skin infections, including bacterial infections such as styes, boils, and infections of hair follicles, as well as fungal infections such as athlete’s foot and ringworm.
Understanding these common skin conditions in people with diabetes can help in early detection and treatment. In the following sections, we will discuss how to prevent and treat these conditions.
Preventing Skin Conditions in People with Diabetes
Preventing skin conditions in people with diabetes primarily involves managing blood sugar levels and maintaining a good skincare routine. Here are some tips:
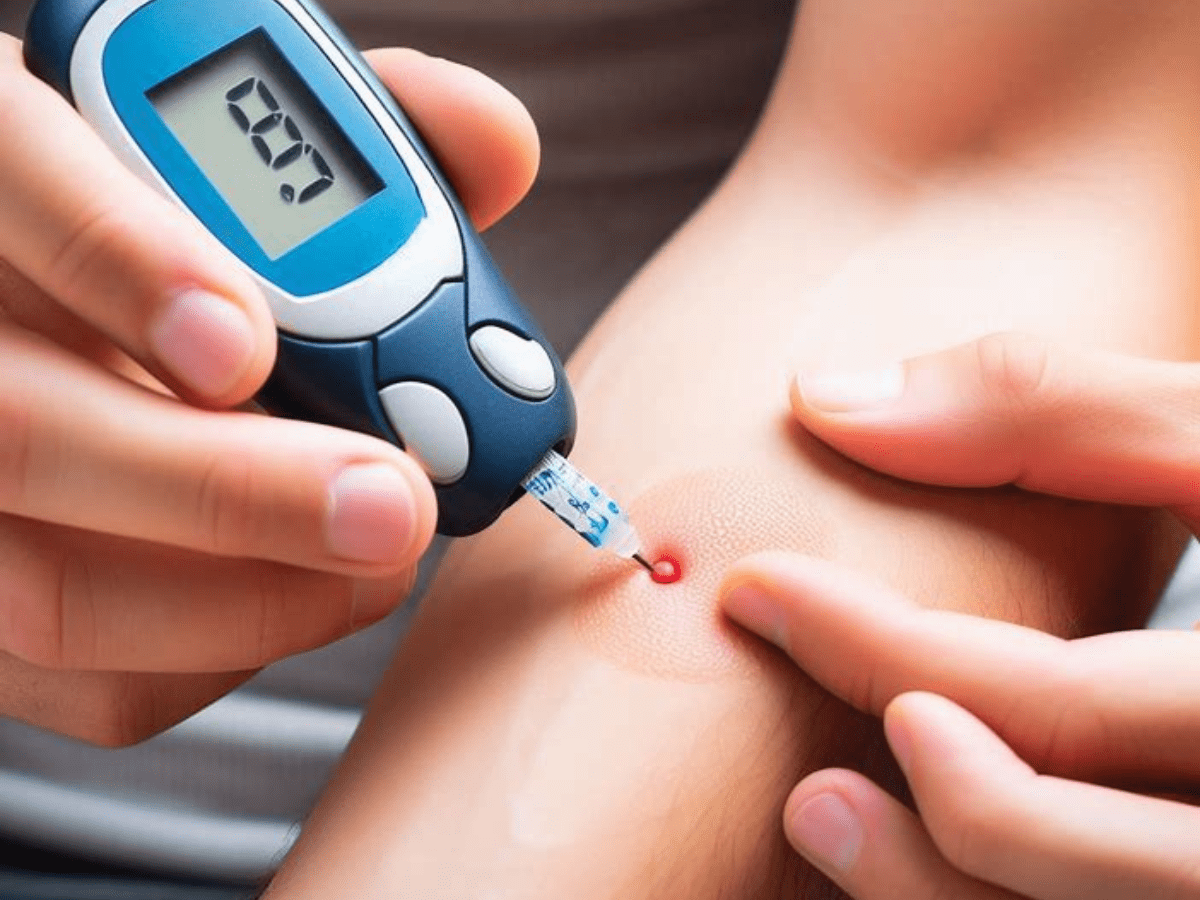
- Control Blood Sugar: You can lessen the risk of skin issues by maintaining blood sugar levels within the range that your doctor has prescribed.
- Skin Care: Keep your skin clean and moisturized. Use mild soaps and lotions that are designed for sensitive skin.

- Stay Hydrated: Drink plenty of fluids to keep your skin hydrated from the inside out.
- Healthy Diet: Eating a balanced diet can help maintain healthy skin. Include foods rich in omega-3 fatty acids, vitamins A, C, and E, and other nutrients that promote skin health.

- Regular check-ups: Regularly check your body for any changes in your skin, especially in places that are hard to see. This can help in the early detection of skin conditions.
Remember, the key to preventing skin conditions in people with diabetes is regular care and early detection. In the following sections, we will discuss how to treat these conditions if they do occur.
Treatment Options for Skin Conditions in People with Diabetes

The treatment for skin conditions in people with diabetes varies depending on the specific condition. Here are some general treatment options:
- Topical Treatments: These are creams, ointments, or lotions applied directly to the skin. They can help treat a variety of skin conditions, including bacterial and fungal infections and inflammatory conditions like eczema.
- Oral Medications: For more severe skin conditions or those that don’t respond to topical treatments, oral medications may be prescribed. These can include antibiotics for infections or drugs to reduce inflammation.
- Light Therapy: Some skin conditions, such as psoriasis, may be treated with light therapy, also known as phototherapy. This process entails subjecting the skin to specific forms of illumination.
- Good Skincare Routine: Maintaining a good skincare routine can help manage many skin conditions. This includes keeping the skin clean and moisturized, avoiding harsh soaps, and protecting the skin from the sun.
- Managing Blood Sugar Levels: As high blood sugar levels can contribute to skin conditions, managing your diabetes effectively is a crucial part of treatment.
Remember, if you have diabetes and are experiencing skin conditions, it’s important to consult with a healthcare professional for an accurate diagnosis and treatment plan.
Personal Stories
Personal stories can provide a unique perspective on the experience of living with diabetes and skin conditions. They can offer insight, inspire others, and create a sense of community. Here are a few fictional examples:
- John’s Journey with Type 2 Diabetes and Acanthosis Nigricans: John, a 45-year-old man with Type 2 diabetes, noticed dark, velvety patches on his neck and underarms. After a visit to his dermatologist, he was diagnosed with acanthosis nigricans. With a combination of topical treatments and better management of his diabetes, John saw a significant improvement in his skin condition.
An image here showing a person’s journey could help readers visualize this story.
- Sarah’s Struggle with Type 1 Diabetes and Diabetic Dermopathy: Sarah, a young woman with Type 1 diabetes, started noticing light brown, scaly patches on her legs. She learned that this was diabetic dermopathy, a harmless condition common in people with diabetes. Sarah shares how she manages her skin condition along with her diabetes.
- Mike’s Experience with Type 2 Diabetes and Skin Infections: Mike, who has Type 2 diabetes, had recurring skin infections. He shares his story of how he overcame these infections with a combination of medications and a good skincare routine.
These stories highlight the experiences of people living with “diabetes and skin conditions,” emphasizing the importance of early detection, effective management, and the impact of these conditions on individuals’ lives.
Conclusion and Summary
In this blog post, we’ve explored the complex relationship between diabetes and skin conditions. We’ve learned that diabetes, a chronic health condition that affects how your body turns food into energy, can have significant effects on the skin. This can lead to a variety of skin conditions, some of which are unique to people with diabetes.
We’ve delved into some of the most common skin conditions that people with diabetes may experience, including diabetic dermopathy, necrobiosis lipoidica diabeticorum, and diabetic blisters. We’ve also discussed the importance of preventing these conditions through managing blood sugar levels, maintaining a good skincare routine, staying hydrated, eating a healthy diet, and having regular check-ups.
Treatment options for these skin conditions vary, but they often involve topical treatments, oral medications, light therapy, a good skincare routine, and effective management of diabetes.
We’ve also shared personal stories of people living with diabetes and skin conditions, highlighting the importance of early detection, effective management, and the impact of these conditions on individuals’ lives.
Remember, if you have diabetes and are experiencing skin conditions, it’s important to consult with a healthcare professional for an accurate diagnosis and treatment plan. With the right care and management, people with diabetes can lead healthy lives and effectively manage their skin health.
References
This blog post was created using a variety of resources to ensure accurate and up-to-date information. Here are some of the key references used:
- American Diabetes Association. (2023). Living with Diabetes: Skin Complications. Retrieved from Website Name
- Mayo Clinic. (2023). Diabetes and Skin Conditions: What’s the Connection? Retrieved from Website Name
- Institute for Diabetes, Digestive, and Kidney Health (2023). Preventing Diabetes Problems: Skin Complications. Retrieved from Website Name
- WebMD. (2023). Skin conditions in diabetes. Retrieved from Website Name
Please note that while we strive to keep the information in this post up to date and correct, we make no representations or warranties of any kind about the completeness, accuracy, reliability, suitability, or availability of any information, products, services, or related graphics contained in this post for any purpose.
Remember to replace the website name with the actual URLs of the sources you used. It’s important to cite all the sources of information used in the blog post to give proper credit and provide readers with additional resources to learn more about diabetes and skin conditions.
Please note that the actual references you use may vary depending on the sources of your information. Always ensure to use reliable and up-to-date sources to maintain the credibility and accuracy of your blog post.
FAQ
Q: Can diabetes cause rashes or itching?
Yes, diabetes can cause dry skin, leading to itching. Additionally, nerve damage from diabetes can trigger itching sensations without a visible rash.
Q: Are skin conditions always a sign of diabetes?
Not necessarily. While some skin conditions are more common among individuals with diabetes, they can occur due to various reasons unrelated to diabetes.
Q: Can diabetic skin conditions be cured?
While certain diabetic-related skin conditions can be managed effectively, a complete cure might not always be possible. However, proper management and care can significantly alleviate symptoms.
Q: Can diabetes medications affect the skin?
Some diabetes medications may have side effects that impact the skin, such as increased sensitivity to sunlight or allergic reactions. Always consult your healthcare provider if you notice any changes.
Q: Does controlling blood sugar help with skin conditions?
Maintaining stable blood sugar levels is essential to managing and preventing various skin issues associated with diabetes.
Q: How often should one get their skin checked if they have diabetes?
Regular skin checks are advisable, ideally during routine visits to your healthcare provider. However, if you notice any unusual changes, seek medical attention promptly.
Q: Are there specific skincare products recommended for people with diabetes?
Using mild, fragrance-free moisturisers and cleansers is generally recommended. However, consulting a dermatologist for personalised recommendations is advisable.
Q: Can diabetes cause skin discoloration?
Yes, conditions like acanthosis nigricans can cause dark, velvety patches in body folds, often associated with insulin resistance in diabetes.
Q: Are diabetic skin infections serious?
Diabetic-related skin infections can escalate if not treated promptly. It’s crucial to seek medical attention for a proper diagnosis and treatment.
Q: Does a healthy diet impact diabetic skin conditions?
Yes, a balanced diet can positively impact skin health with diabetes. Nutrient-rich foods contribute to overall well-being, reflecting on the skin as well.
N.B. This article provides insights into the relationship between diabetes and skin conditions. For specific concerns or advice, consult with a healthcare professional.