Last Updated on January 30, 2024 by Alexander Sennuga
Find below a discussion on diabetes foot facts, curated from scientific sources. Furthermore, the information is gathered through intensive research on the subject.
As we know, diabetes is a disease that is currently spreading globally at an alarming rate. It’s a disease that leads to complications if not treated early and well.
One of the effects of negligence in treating the disease is foot pain. Thus, diabetics may well be afflicted with foot problems. This problem can occur in the two common types of diabetes. That is, in types 1 and 2.
What is the science behind these foot problems? Are there steps diabetics can take to reduce the risk? So, if yes, what are they?
This post will attempt to provide the answers to the above questions.
And then many more…
Let’s go.
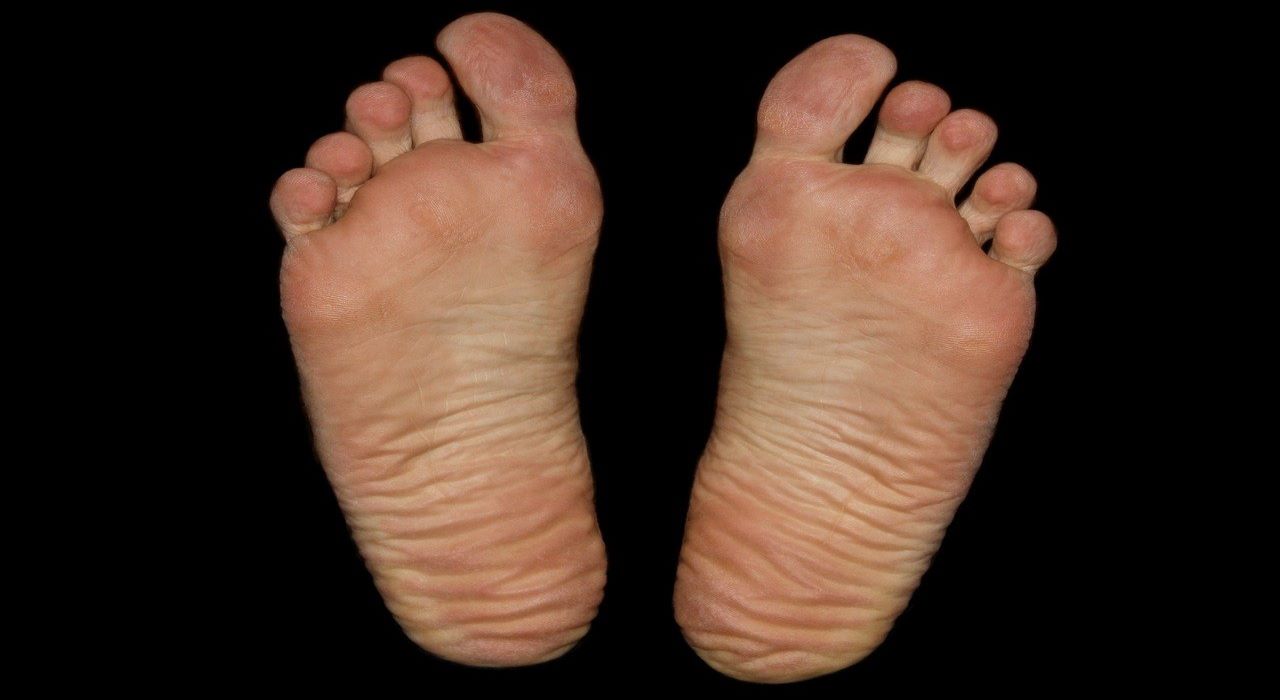
What is a diabetic foot?
When diabetes is not well controlled, damage to the organs and impairment of the immune system is likely. Foot problems commonly develop in people with diabetes and can quickly become serious. With damage to the nervous system, a person with diabetes may not be able to feel his or her feet properly.
Normal sweat secretion and oil production that lubricate the skin of the foot are impaired. These factors together can lead to abnormal pressure on the skin, bones, and joints of the foot during walking and can lead to a breakdown of the skin of the foot. Damage to blood vessels and impairment of the immune system from diabetes make it difficult to heal these wounds.
Bacterial infection of the skin, connective tissues, muscles, and bones can then occur. These infections can develop into gangrene. Because of the poor blood flow, antibiotics cannot get to the site of the infection easily. Often, the only treatment for this is amputation of the foot or leg. If the infection spreads to the bloodstream, this process can be life-threatening.
Source: [The HealthSite.com]
How does diabetes cause foot problems?
As a result of long-term high blood glucose, diabetes-related leg complications can occur. One such complication is called diabetic neuropathy, or simply nerve damage. This is one of the diabetes foot facts.
Diabetic neuropathy represents the most common cause of numbness in the legs. Untreated type 2 diabetes usually results in this ailment.
How does this problem occur?
People with long-standing or poorly controlled diabetes are at risk of having damage to the nerves in their feet. Because of the nerve damage, the patient may be unable to feel their feet normally. Also, they may be unable to sense the position of their feet and toes while walking and balancing.
With normal nerves, a person can usually sense if their shoes are rubbing on the feet or if one part of the foot is becoming strained while walking. A person with diabetes may not properly sense minor injuries (such as cuts, scrapes, and blisters), signs of abnormal wear and tear (that turn into calluses and corns), and foot strain.
Normally, people can feel if there is a stone in their shoe and then remove it immediately. A person who has diabetes may not be able to perceive a stone. Its constant rubbing can easily create a sore.
Source: [The HealthSite.com]
Type 2 Diabetes Foot Problems
Both type 1 and type 2 diabetes cause damage to blood vessels and peripheral nerves, which can result in problems in the legs and feet. Two main conditions, 1) peripheral artery disease (PAD) and 2) peripheral neuropathy, are responsible for the increased risk of foot problems in people with diabetes.
- Peripheral artery disease (PAD), sometimes referred to as peripheral vascular disease (PVD), means that there is narrowing or occlusion by atherosclerotic plaques of arteries outside of the heart and brain. This is sometimes referred to as the “hardening” of the arteries. Diabetes is a known risk factor for developing peripheral artery disease.
- In addition to pain in the calves during exercise (medically known as intermittent claudication), the signs and symptoms of peripheral artery disease relate to a decreased delivery of oxygen to the lower legs and feet.
- Peripheral neuropathy refers to damage to the peripheral nerves directly as a result of diabetes. Symptoms of peripheral neuropathy include decreased sensation in the nerves of the legs and feet, making it difficult to perceive injuries due to a lack of feeling. Peripheral neuropathy also causes tingling, pain, or burning in the involved areas.
- It can also cause the muscles of the feet to work improperly, leading to misalignment of the foot that can put pressure on certain areas of the foot.
Source: (medicinet.com)
What are diabetes foot risk factors?

Several factors often influence this nerve damage, and they include the following:
- How long the diabetic has been suffering from diabetes?
- Age of the diabetes patient
- Smoking
- High blood pressure
- High cholesterol
- Vitamin B12 deficiency
- Heavy alcohol consumption
- Slow metabolism
Forms of Neuropathy and Their Characteristics
In broad terms, there are two forms of neuropathy. What are they? The first one is known as autonomic neuropathy of the legs. The other is sensory polyneuropathy. The two will be described below.
Autonomic neuropathy of the legs
This is another one of the diabetes foot facts.
Each time neuropathy is to occur, it starts with autonomic neuropathy. How? The following become noticeable:
- Feet sweating will cease
- There is dryness of the feet
- The hair on the feet will disappear
- Nerves that control the blood flow to the small blood vessels in the skin are affected
- A sense of cold feet but warmth when touched. Why? This is due to an increase in the blood flow to medium-sized blood vessels.
- Lack of oxygen and drying of the skin
- Tightening of shoes prevents blood flow to the feet, which causes discomfort
- The dryness of the legs causes deep cracks in the skin, especially on the heels. This can lead to foot wounds
Sensory polyneuropathy
This is also one of the diabetes foot facts.
This is a form of neuropathy that has the characteristic of affecting the sensory nerves. It is these nerves that send signals from the skin, bones, and muscles to the brain.
This form of neuropathy affects the senses; hence, they show symptoms compared to the other form mentioned earlier. So, this makes it the most common neuropathy.
The usual symptoms include the following:
- Burning
- Toothache-like pain
- Tingling
- Sweating
- Electric-like sensations
These symptoms often get worse at night and may prevent sound sleep. But there is often relief after getting up and walking.
The good news is that treatment is often available for the pain. However, sufferers need to contact their doctor for help with the above symptoms. There’s no need to delay asking for help, thus allowing the situation to get worse.
Diabetes foot facts: Can diabetic feet be prevented?
A person with diabetes should do the following:
- Foot examination: Examine your feet daily and also after any trauma, no matter how minor, to your feet. Report any abnormalities to your doctor. Use a water-based moisturiser every day (but not between your toes) to prevent dry skin and cracking. Wear cotton or wool socks and avoid elastic socks and hosiery because they may impair circulation
- Eliminate obstacles: Move or remove any items you will likely trip over or bump your feet on. Keep clutter on the floor picked up
- Toenail trimming: Always cut your nails with a nail cutter and not any other device. Cut them straight across and leave plenty of room out from the nail bed or quickly. If you have difficulty with your vision or using your hands, let your doctor do it for you or train a family member how to do it safely
- Footwear: Wear sturdy, comfortable shoes whenever feasible to protect your feet. To be sure your shoes fit properly, see a podiatrist (foot doctor) for fitting recommendations or shop at shoe stores specialising in fitting people with diabetes. If you have flat feet, bunions, or hammertoes, you may need prescription shoes or shoe inserts
- Exercise: Regular exercise will improve bone and joint health in your feet and legs, improve circulation to your legs, and will also help to stabilise your blood sugar levels. Consult your doctor before beginning any exercise program.
- Smoking: If you smoke, quitting can be one of the best things you can do to prevent problems with your feet. Smoking accelerates damage to blood vessels, especially small blood vessels, leading to poor circulation, which is a major risk factor for foot infections and ultimately amputations.
- Diabetes control: following a reasonable diet, taking your medications, checking your blood sugar regularly, exercising regularly, and maintaining good communication with your doctor are essential to keeping your diabetes under control. Consistent long-term blood sugar control to near-normal levels can greatly lower the risk of damage to your nerves, kidneys, eyes, and blood vessels
People with diabetes must be fully aware of how to prevent foot problems before they occur, recognise problems early, and seek the right treatment when problems do occur.
Although treatment for diabetic foot problems has improved, prevention, including good control of blood sugar levels, remains the best way to prevent diabetic complications. People with diabetes should learn how to examine their own feet and how to recognise the early signs and symptoms of diabetic foot problems.
They should also learn what is reasonable to manage routine at-home foot care, how to recognise when to call the doctor, and how to recognise when a problem has become serious enough to seek emergency treatment.
Source: [The HealthSite.com]
Right Treatment for Diabetes Foot Problems

There are three stages to the treatment of the diabetic foot.
The first step is debridement, which is the process of removing all the dead and dying tissue from the area. It also involves cleaning the area well and cleaning out any pus that may be present.
The second step is drainage. This is mainly for wounds that have pus in them. It has been found that only treating the wound with antibiotics does not help with diabetes.
Proper and timely drainage has helped several people retain their limbs.
The third step is bandaging and infection control. This is the process of bandaging the wound properly and treating the patient with appropriate antibiotics.
After this procedure, the patient is required to take care of the wound until it heals. It is advised that a patient not put any weight on the region; this can cause further spread of the condition.
There are times when a small ulcer on the foot can become gangrenous. This is a condition where the wound becomes infected and the skin and tissue start to die due to the infection. This condition comes about if the patient has ignored a non-healing ulcer for a long time.
In such cases, a doctor may suggest amputating the limb. The extent to which the limb will be amputated depends on how far the gangrene has spread.
Source: [The HealthSite.com]
Is there anything else to do in this regard?
See below.
How To Control Type 2 Diabetes Foot Pain
The best prevention for nerve pain, ultimately, is to manage your diabetes well. A 2006 study by the National Institute of Diabetes and Digestive and Kidney
Diseases showed that strict blood glucose control with intensive insulin therapy lowered the chances in people with type I (insulin-requiring) diabetes of having symptoms of peripheral neuropathy — tingling, burning, and pain — by 64%.
These results have also been shown to hold in type II diabetes, too.
The two most important determinants of whether you get diabetic neuropathy are how many years you have had diabetes and how well you control your blood sugar. Other factors, including controlling blood pressure and blood fats (cholesterol and triglycerides) and not smoking, are also important to prevent diabetic neuropathy.
These are diabetes foot facts that are well-known.
Controlling your blood glucose also helps reduce the symptoms of diabetic nerve pain. So the good news is that controlling your glucose levels with diet, exercise, and, if needed, medications can not only help prevent diabetic peripheral neuropathy, but they can also help ease its effects.
Source: (medicinenet.com)
Extra things to do to treat diabetes foot
It is advisable to ensure the following gets your attention:
- Avoid walking barefoot, but always protect your feet
- Only wear the appropriate type of shoes. And seek advice on this from your doctor, if necessary
- Visit your foot control support regularly
- Pay attention to any impaired feet’ senses and seek assistance if you notice any issues
- Request support if you notice any unusual changes in your legs
- Stop or avoid smoking
- Engage in moderate exercise to promote blood flow to the legs and feet
Conclusion
Over time, prolonged diabetes, type 1 or type 2, can lead to foot problems. There are two main types of complications within the foot. These are diabetic neuropathy (nerve damage) and vascular disease. These are diabetes foot facts.
Diabetic neuropathy has two forms. We have the autonomic form, which normally occurs first. The other form is what is called sensory polyneuropathy.
There are many risk factors for this disease, among which are the age of diabetes and how long diabetes has existed. Others are heavy alcohol consumption, high blood pressure, and high cholesterol.
There are a number of steps to take for the treatment of foot problems. The major one is a regular examination of the feet, possibly daily. You must check for swelling, discoloration, redness, and the temperature of the feet.
Moreover, you must report unusual situations to your doctor or other healthcare providers.
Besides the routine checks and reporting unusual signs for help mentioned above, some lifestyle changes are vital. What are these? Walking barefoot is bad for you, so it is smoking.
You need to put on only the right kind of shoes and seek advice from your doctor if need be. You need to visit your foot control/support team for regular check-ups. Engaging in moderate exercise regularly is often helpful.
Why? This will enhance blood flow to the legs and feet.
FAQ
**Q: What are some important facts about diabetes foot care?
A: Diabetes foot care is crucial for individuals with diabetes to prevent complications. Here are some important facts to keep in mind:
– People with diabetes are more prone to foot problems due to poor circulation and nerve damage.
– Regularly inspect your feet for any cuts, blisters, or sores, and seek medical attention if you notice any abnormalities.
– Wash your feet daily with warm water and mild soap, thoroughly drying them, especially between the toes.
– Moisturize your feet to prevent dryness and cracking, but avoid applying lotion between the toes.
– Trim your toenails straight across to prevent ingrown nails, and have them professionally trimmed if needed.
– Wear well-fitting, comfortable shoes and socks that allow your feet to breathe. Avoid going barefoot.
– Check your shoes for foreign objects or rough areas that could cause irritation or injury.
– Engage in regular physical activity to improve circulation, but consult your doctor before starting any exercise program.
– Quit smoking, as it impairs blood flow to the feet and increases the risk of complications.
– Schedule regular foot exams with a healthcare professional to monitor your foot health.
**Q: What are the symptoms of diabetic foot problems?**
A: Diabetic foot problems can exhibit various symptoms, including:
– Numbness or tingling sensation in the feet.
– Loss of feeling in the feet.
– Changes in skin colour or temperature.
– Swelling or inflammation.
– Foot ulcers or sores that are slow to heal.
– Ingrown toenails or fungal infections.
– Pain or cramping in the legs.
– Changes in the shape of the feet or toes.
– Foot deformities.
If you experience any of these symptoms, it’s important to seek medical attention promptly to prevent further complications.
Q: How can individuals with diabetes prevent foot ulcers?
A: Preventing foot ulcers is crucial for individuals with diabetes. Here are some preventive measures:
– Inspect your feet daily for any signs of redness, blisters, sores, or cuts.
– Keep your feet clean and dry, ensuring to thoroughly dry between the toes.
– Moisturise your feet with lotion, but avoid applying it between the toes.
– Trim your toenails straight across and avoid cutting them too short.
– Wear well-fitting, comfortable shoes and socks that protect your feet.
– Avoid going barefoot, especially in public places.
– Check your shoes for foreign objects before wearing them.
– Protect your feet from extreme temperatures and avoid exposing them to hot surfaces.
– Engage in regular physical activity to improve blood circulation.
– Control your blood sugar levels and follow a healthy lifestyle.
If you notice any foot abnormalities or have concerns, consult a healthcare professional for appropriate care and guidance.
Q: How often should individuals with diabetes check their feet?
A: Individuals with diabetes should check their feet daily. Regular foot inspections help identify any changes or abnormalities early on. It’s important to examine the entire foot, including the top, bottom, heels, between the toes, and toenails.
If you have difficulty inspecting your feet, use a mirror or seek assistance from a family member or caregiver.
In addition to daily self-exams, it’s recommended to have a professional foot examination by a healthcare provider at least once a year or as advised by your healthcare team.
**Q: Are there specific footwear recommendations for individuals with diabetes?
A: Yes, there are specific footwear recommendations for individuals with diabetes to maintain foot health:
– Choose shoes that provide proper support and comfort, with cushioning and a wide toe box.
– Opt for shoes made of breathable materials to allow air circulation.
– Look for shoes with adjustable closures, such as Velcro or laces, to ensure a secure fit.
– Avoid high heels, pointed-toe shoes, and shoes that are too tight or narrow.
– Consider wearing diabetic shoes or orthotic inserts to provide extra support and cushioning.
– Wear moisture-wicking socks made of natural fibers to keep your feet dry.
– Avoid tight or restrictive socks that can impair circulation.
– Change your socks daily and whenever they become damp.
– Inspect your shoes for rough seams, foreign objects, or any signs of wear and tear.
– Consult a podiatrist or footwear specialist for personalised advice and recommendations based on your specific foot needs.
Remember, proper footwear plays a vital role in preventing foot complications for individuals with diabetes.
Do you have additional information about diabetes foot problems? Please share them in the comments section.
Very Important: Please note that each piece of information we provide on this site is for educational purposes only. They’re not for medical advice, diagnosis, or treatment.
So, please consult your doctor and/or a registered dietitian or nutritionist for any professional advice. Hence, do that before applying the knowledge to your health issues.